From 3rd – 7th October, it is a time to showcase and celebrate Physician Associates (PAs) – what they do, why they do it, and importantly how they support the NHS. The aim of Physician Associate Week is to raise awareness of this new and exciting profession in the field of medicine.
Who are Physician Associates?
Physician Associates are healthcare professionals with a generalist medical education who work alongside doctors, nurses, and other healthcare professionals as part of the multidisciplinary team. They are dependent practitioners working with a dedicated supervisor, but are able to work autonomously with appropriate support.
What do Physician Associates do?
Physician Associates are able to:
- Take medical histories from patients.
- Carry out physical examinations.
- See patients with undifferentiated diagnoses and long-term chronic conditions.
- Formulate differential diagnoses and management plans.
- Perform diagnostic and therapeutic procedures.
- Develop and deliver appropriate treatment and management plans.
- Request and interpret diagnostic studies.
- Provide health promotion and disease prevention advice for patients.
Physician Associates are currently not able to:
- Prescribe
- Request ionising radiation (e.g. chest x-ray or CT scan).
- Provide care or treatments to patients in an unsupervised setting.
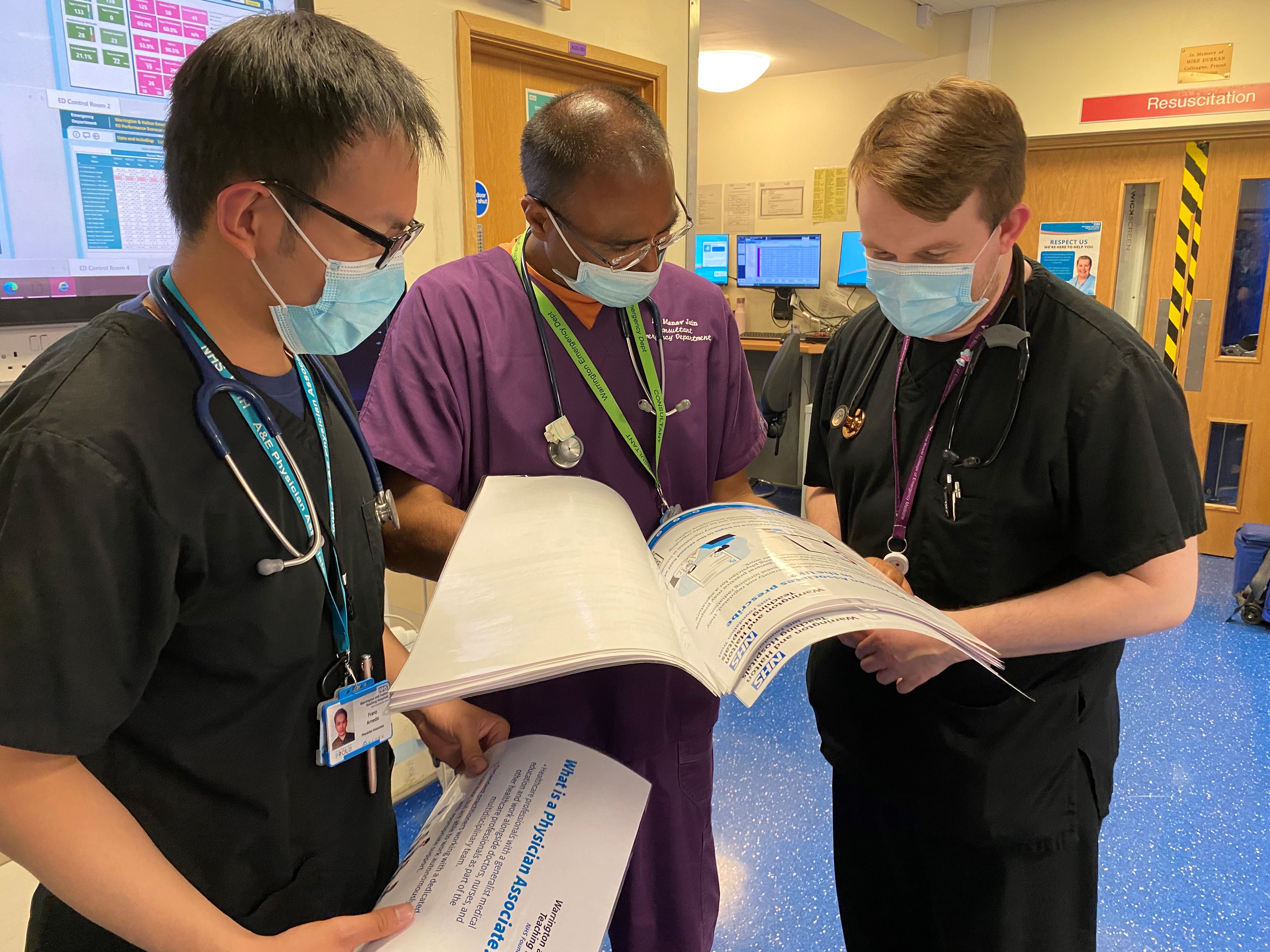
Physician Associates at Warrington Hospital
Currently, there are 18 Physician Associates who work at Warrington Hospital: 12 work in the Emergency Department, two in General Surgery, one in Paediatrics, two in the Frailty Assessment Unit, and one in the Geriatric ward, as well as four more locum PAs.
At Warrington Hospital, Physician Associate students from the University of Chester gain experience in various departments such as Trauma & Orthopaedics, Endocrinology, Cardiology, Respiratory, Stroke, Acute Medical Unit, Obstetrics & Gynaecology, Paediatrics, General Surgery and A&E.
At the end of each month, there is a designated day that allows all the PAs from the hospital to meet and give feedback on their progress as well as to provide teaching opportunities for each other to sustain their professional development. These teaching sessions may involve seminars and even simulated scenarios alongside doctors, nurses, and clinical educators.
All the PAs at the trust are assigned a clinical supervisor who have a responsibility for their ongoing development including appraisals and professional development plans. Supervision is similar to that of junior or trust grade doctors and levels of supervision will vary based on many factors such as their past healthcare experience or years of experience as a Physician Associate.
In the 1960s, physicians and educators recognised a shortage of primary care physicians after World War II. Therefore, to help improve and expand healthcare, Dr Eugene A. Stead Jr. put together the first class of PAs in 1965. He selected four Navy Hospital Corpsmen who had received considerable medical training during their military service. Stead based the curriculum of the PA programme on his knowledge of the fast-track training of doctors during World War II.
On 6th October 1967, the first PA class graduated from the Duke University PA programme and PAs have since been an integral part of the USA healthcare system, with approximately 140,000 qualified PAs. In 1980, PAs in the USA were given prescribing authority in 10 states and since 2007, PAs have prescribing rights in all 50 states.
In the UK, PAs are managed on a voluntary register by the Faculty of Physician Associates (FPA) and they are currently unable to prescribe without statutory regulation. However, there are ongoing discussions with the General Medical Council (GMC) which maintains the official register of doctors to regulate Physician Associates. Talks about regulation within parliament are expected to begin in 2023 and GMC regulation is expected to take place in 2024 at the earliest. Once regulated, there may be possible discussions about PA prescribing rights.

Currently in the UK, there are 38 postgraduate and two undergraduate Physician Associate Studies courses. Primarily to qualify as a Physician Associate, candidates must complete a 2-year MSc Physician Associate Studies course which focuses principally on general medicine in hospital and general practice.
Prior to joining the course, candidates are required to have graduated with a minimum 2:1 classification from a 3-year Bachelor of Science degree. Many have previous healthcare experience such as being nurses, pharmacists, biomedical scientists, or physiotherapists etc.
The course is split into approximately 50% theory and 50% practical blocks in which Physician Associate students are expected to complete a minimum of 1,600 placement hours as part of their training which covers: community medicine 510 hours, general hospital medicine 350 hours, emergency medicine 180 hours, general surgery 90 hours, obstetrics & gynaecology 90 hours, paediatrics 90 hours, mental health 90 hours, and the remaining are covered through training simulations.
Upon successful completion of their course by passing their university exams, they must take the Physician Associate National Exam (PANE) to be registered on the Physician Associate Managed Voluntary Register (PAMVR) and receive their license to practise medicine.
These National Exams consist of a written paper and Objective Structured Clinical Examinations (OSCEs) which test the candidates on their clinical skills, knowledge, and attitude through a series of intense patient-simulated 14 stations. These exams test the candidates across all specialities.
On top of all that, they are required to take a recertification exam every 6 years to retain their license and keep up-to-date with their clinical skills and knowledge.

As of 2022, at least sixteen countries utilise Physician Associates/Assistants in their healthcare systems, including USA, UK, Canada, Germany, Netherlands, and Australia.
In the UK, there are approximately 3,200 practising Physician Associates who are based in hospitals, general practices, and mental health wards.
Physician Associates bring new talent to the healthcare system and can provide vital support to patients and the multidisciplinary team which will be necessary for them to be a household name in the NHS for the years ahead.
To learn more about Physician Associates: https:/
https://www.thepalife.com/physician-assistants-pas-and-associates-around-the-world/
https://www.fparcp.co.uk/
https://www.fparcp.co.uk/pamvr/search?search1=&search2=&search3=&search=true
https://www.aapa.org/about/history/
https://www.zippia.com/physician-assistant-jobs/demographics/
https://www.rcpjournals.org/content/futurehosp/9/1/21